Introduction
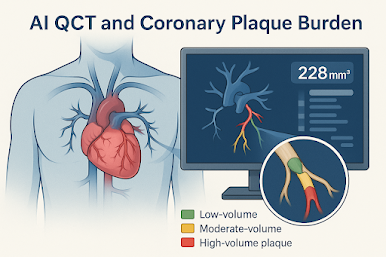
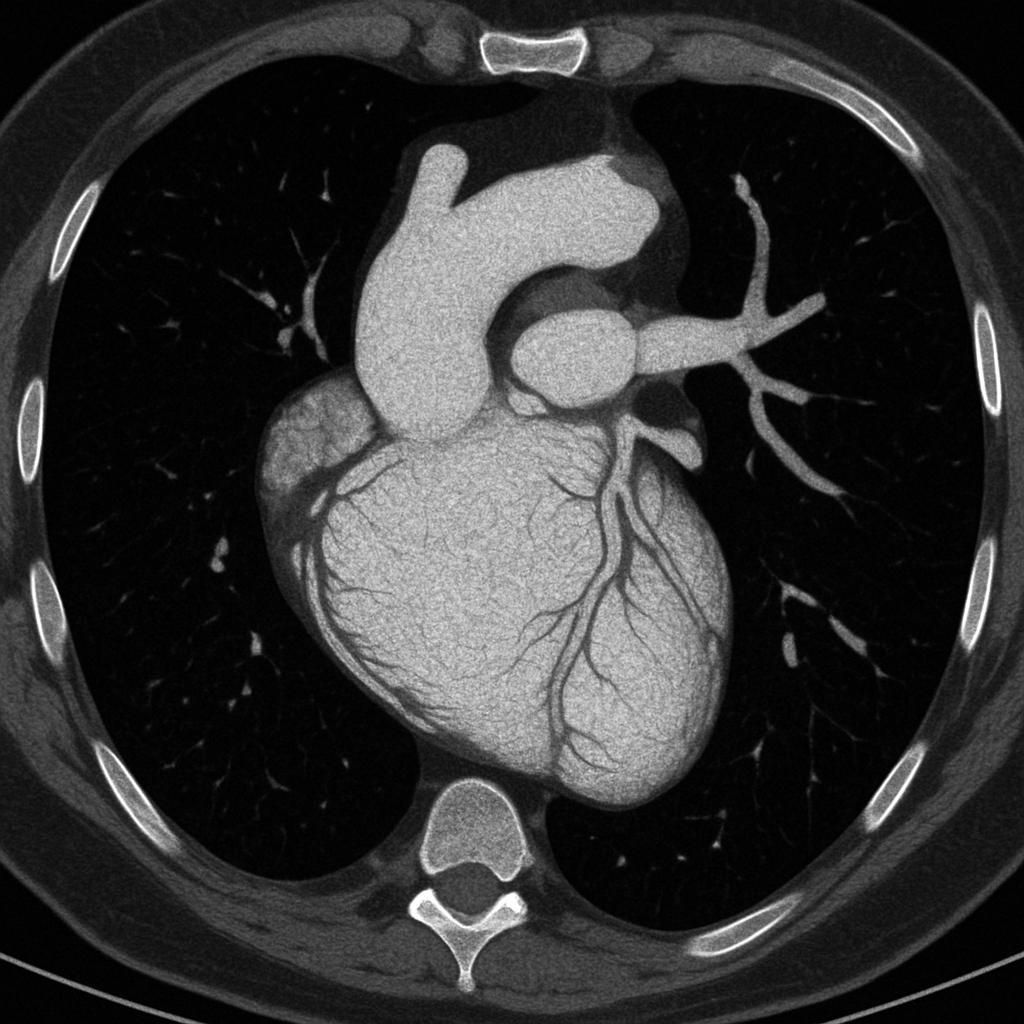
As artificial intelligence (AI) continues to transform cardiovascular diagnostics, its integration into coronary CT angiography (CCTA) is showing compelling promise. The DECIDE registry, presented at the 2025 Society of Cardiovascular Computed Tomography (SCCT) meeting, demonstrates that AI-based coronary plaque analysis (AI-CPA) can lead to meaningful changes in clinical management for over half of symptomatic patients—while simultaneously reducing long-term costs. This marks a significant step forward in personalized cardiovascular prevention and risk stratification.
AI-Driven Insights Go Beyond Stenosis Severity
The DECIDE registry assessed the clinical utility of AI-enabled plaque quantification using a commercial platform (HeartFlow) in 972 symptomatic patients undergoing CCTA. The analysis remained blinded until 90 days post-index CCTA, at which point clinicians were provided AI-derived plaque burden and staging (mild, moderate, severe, or extensive).
-
Primary finding: In 51.3% of patients, AI-CPA led to a change in medical management.
-
Treatment escalations occurred in 36%, including increased statin dosing or new lipid-lowering therapy.
-
Management changes were more frequent in patients with higher plaque burden, diabetes, hypertension, hyperlipidemia, and CT-FFR < 0.80.
This demonstrates how quantitative plaque analysis, independent of luminal stenosis, can recalibrate treatment intensity more effectively than risk calculators alone.
Better LDL Targeting and Lipid Control
In patients whose management changed, 44.1% started a new lipid-lowering agent, while 23.5% had dosage intensifications. Among those with serial cholesterol testing, significant improvements in LDL and HDL were observed only in patients who had management changes (P ≤ 0.01), reinforcing the downstream effect of AI-informed care on biomarkers and adherence.
Visualizing Disease for Patients and Providers
Physicians noted that AI-generated arterial images helped bridge the gap between diagnosis and behavior change, facilitating shared decision-making. Presenting visual evidence of coronary plaque, LDL targets, and personalized risk empowered patients to better understand their disease and adhere to medication.
“It simplifies the discussion into one or two sentences. Showing patients their actual arteries and plaque burden improves compliance,” one investigator noted.
Real-World Economic Value: $719 Saved Per Patient Over 10 Years
Using Medicare fee-for-service data from the FISH&CHIPS study, a cost-effectiveness model projected:
-
All-cause mortality reductions of 0.3% to 1.1% over 3.5 to 10 years.
-
Cost savings per patient of:
-
$263 at 3.5 years
-
$373 at 5 years
-
$719 at 10 years
-
These projections assume a one-time AI-CPA cost of $950 and account for downstream healthcare expenditures including PCI, ambulance transport, and inpatient care. Despite increased use of statins or PCSK9 inhibitors, the model suggests that upfront investments in AI-CPA are justified by lower event rates and hospitalizations.
Implications for Clinical Practice and Future Research
The DECIDE registry supports the growing sentiment that AI-augmented CCTA may soon redefine preventive cardiology. While long-term outcome trials are underway, the current findings suggest that quantifying coronary plaque offers actionable intelligence beyond traditional metrics.
"This isn’t just about plaque detection; it’s about precision therapy and early intervention," experts said. "We're witnessing the convergence of imaging and lipidology."
Key Takeaways for Busy Clinicians
-
AI-based coronary plaque analysis (AI-CPA) changed management in over 50% of symptomatic patients post-CCTA in the DECIDE registry.
-
Changes included new or intensified lipid-lowering therapies, which translated to better cholesterol control.
-
AI-CPA improved patient engagement and provided a visual tool to guide shared decisions.
-
Cost-modeling studies suggest $719 per patient savings over 10 years, despite the initial cost of AI analysis.
-
These findings support broader adoption of AI-enhanced plaque staging to guide personalized secondary prevention.
References
.png)