🌟 A New Frontier in Prevention
A quiet revolution in cardiology took shape at the AHA 2025 Scientific Sessions and in the pages of the New England Journal of Medicine.
The VESALIUS-CV trial is the first to show that a PCSK9 inhibitor — evolocumab (Repatha; Amgen) — can prevent first major cardiovascular events in people who have never had a heart attack or stroke.
It signals a shift from treating damage to preventing disease altogether — a milestone for lipid management.
🧪 Inside the VESALIUS-CV Trial
12,257 patients, all at high cardiovascular risk but with no prior MI or stroke, were randomized to evolocumab 140 mg every 2 weeks or placebo, on top of statin therapy.
After 4.6 years of follow-up, the results spoke clearly:
💥 Major Outcomes
LDL-C reduction: 55%, to ~45 mg/dL
MACE reduction: 25% (HR 0.75; 95% CI 0.65–0.86)
Expanded endpoint (including revascularization): 19% reduction (HR 0.81)
Safety: No new concerns observed
These findings validate that pushing LDL even lower — near 40 mg/dL — can save lives long before a first event.
🔍 How It Differs from Earlier Trials
Earlier studies such as FOURIER and ODYSSEY Outcomes established PCSK9 inhibitors for secondary preventionafter MI or stroke.
VESALIUS-CV, in contrast, entered unexplored territory — patients with atherosclerosis or high-risk diabetes but no prior events.
It featured:
Higher baseline LDL (~122 mg/dL)
Longer follow-up (4.6 years vs 2.2)
Greater relative and absolute benefit
In essence, it moves PCSK9 therapy upstream, redefining prevention itself.
💡 Clinical Takeaway
For clinicians, this means one thing: don’t wait for the first plaque to rupture.
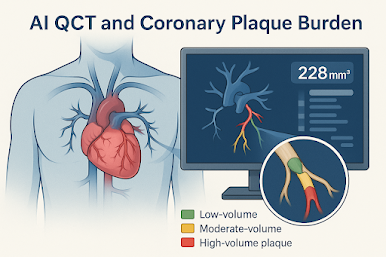
Identify the silent high-risk — those with subclinical CAD, diabetes, PAD, or elevated apoB — and treat aggressively early.
With the FDA’s expanded indication for evolocumab in primary prevention, the data now give physicians stronger footing to act before the first heart attack.
🩺 Key Points for Busy Clinicians
✅ First PCSK9 trial to prove benefit in event-free, high-risk patients
✅ Evolocumab cut MACE by 25%, LDL to ~45 mg/dL, with excellent safety
✅ Longer duration and earlier intervention than prior PCSK9 studies
✅ Supports LDL targets near 40 mg/dL in high-risk, primary-prevention cohorts
✨ The Takeaway:
VESALIUS-CV brings preventive cardiology full circle — proving that aggressive LDL lowering saves lives even before the first event.
The era of “treat early, prevent completely” has begun.

.png)