Introduction
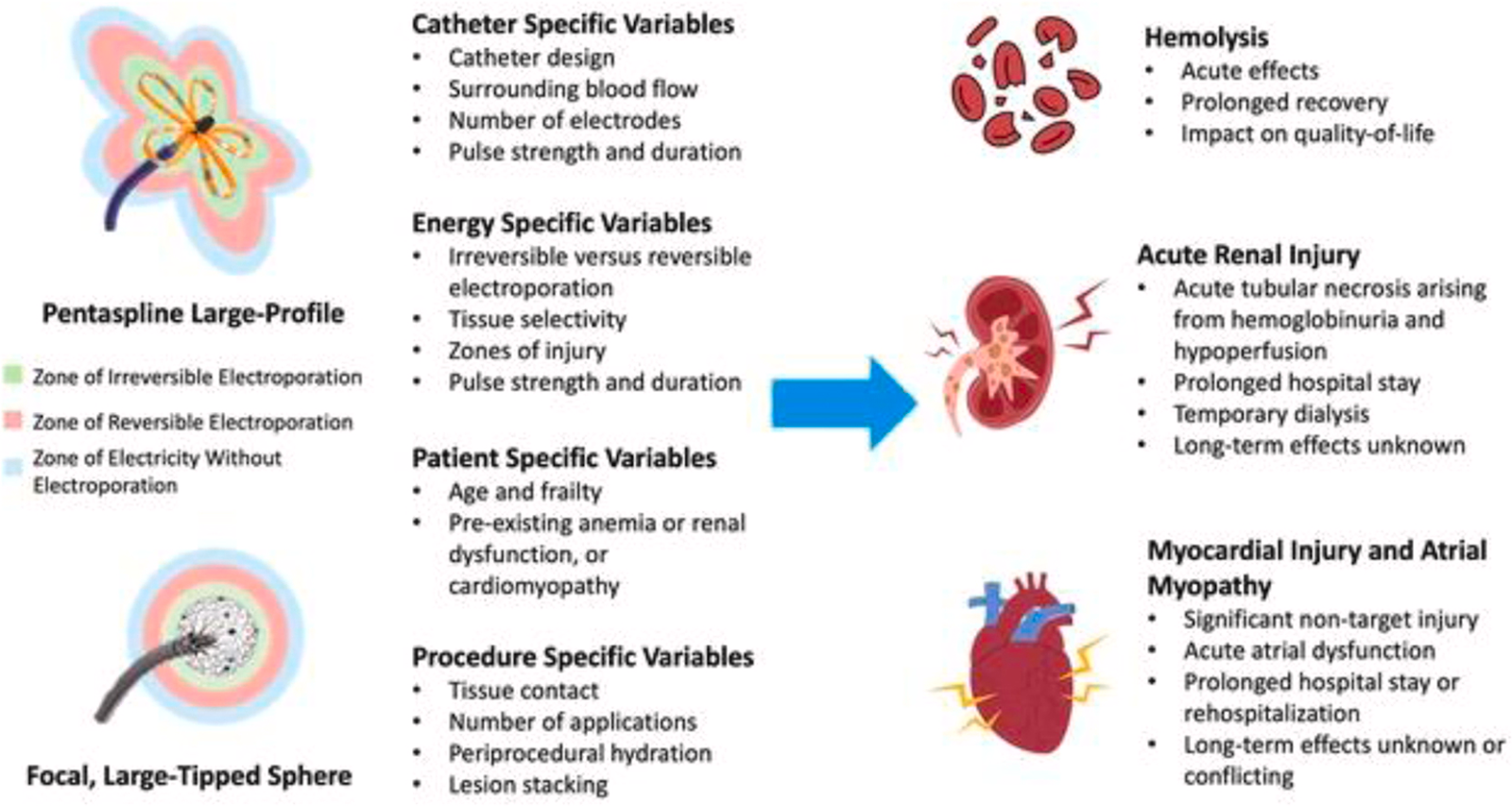
Pulsed-field ablation (PFA) has rapidly emerged as a novel technique for the treatment of atrial fibrillation (AF), offering the potential for tissue-specific ablation with fewer catastrophic complications than traditional thermal methods. However, new data presented at Heart Rhythm 2025 raises concerns about subclinical injury, cerebral embolism, and coronary complications, challenging the narrative that PFA is the “perfect” solution. As the electrophysiology (EP) community embraces this innovation, a deeper understanding of its safety profile is critical.
Safety Signals from the NEMESIS-PFA Registry
The NEMESIS-PFA registry (n=871) compared PFA to radiofrequency ablation (RFA) and identified significantly greater increases in biomarkers of myocardial injury, hemolysis, and renal stress in PFA-treated patients.
-
Cardiac biomarkers like troponin rose substantially higher post-PFA (median: 13,551 vs 128 ng/dL).
-
Indicators of hemolysis—including LDH, haptoglobin, and free hemoglobin—also rose, suggesting red blood cell destruction.
-
Creatinine levels increased more in the PFA group, raising concerns about acute kidney injury.
-
Left atrial ejection fraction (LAEF) dropped more sharply (20% vs 5%), indicating transient atrial dysfunction.
These findings suggest that although PFA avoids esophageal and phrenic nerve injury, it may induce other systemic effects with unclear long-term significance. The biophysical characteristics of PFA catheters—such as electrode geometry, pulse parameters, and electric field strength—likely influence these effects.
🔗 NEMESIS-PFA registry results in JACC: Clinical Electrophysiology
Asymptomatic Cerebral Emboli (ACE): PEACE-AF Findings
In the PEACE-AF study, brain MRI within 72 hours post-PFA revealed asymptomatic cerebral emboli (ACE) in 34% of patients.
-
Older age and persistent AF were associated with increased ACE risk.
-
No clinical stroke or TIA occurred, but long-term neurological outcomes are pending.
While ACE is not unique to PFA, its incidence and potential cognitive implications merit further investigation and systematic surveillance in future trials.
Coronary Complications: Mild but Present
A third study assessed PFA near coronary arteries during cavotricuspid isthmus (CTI) or mitral isthmus ablation. Despite using intracoronary nitroglycerin, 47% of patients developed severe coronary spasm (>70% narrowing).
-
OCT at 3 months showed luminal narrowing and vascular wall thickening, indicating mild coronary stenosis.
-
No patients developed angina or required revascularization, but the data signal a need for vigilance, especially in catheter-specific contexts.
PFA: Still an Evolutionary Technology
Despite these findings, PFA maintains several clear advantages:
-
It avoids atrioesophageal fistula, a rare but often fatal complication of thermal ablation.
-
It is faster, reducing procedure and left atrial dwell time.
-
Some data suggest superior efficacy for rhythm control in select populations.
Ongoing device innovations include dual-mode catheters (e.g., Medtronic’s Sphere-9, capable of both PFA and RFA), which may allow tailored energy delivery based on anatomy and risk.
Expert Perspectives: Caution Over Hype
Experts agree that PFA is a step forward, but not the panacea it's sometimes marketed to be:
-
“We’ve traded one set of major problems for another set of possibly less dire but still significant issues,” said electrophysiologist Dhanunjaya Lakkireddy.
-
“All EPs should understand that PFA is not universally safe, and safety varies by system design,” said Wilber Su.
-
A special issue of Pacing and Clinical Electrophysiology on PFA fundamentals is expected to help standardize operator understanding.
Key Takeaways for Clinicians
-
PFA reduces catastrophic risks like atrioesophageal fistula, but introduces concerns related to myocardial injury, hemolysis, renal dysfunction, and cerebral emboli.
-
Biomarker elevations and drop in atrial function post-PFA highlight a need for longitudinal safety surveillance.
-
ACE incidence post-PFA (34%) supports MRI-based follow-up and neurological assessments in trials.
-
Coronary spasm and stenosis may occur with PFA applied near coronary vasculature, warranting caution in such regions.
-
Future catheter designs should allow selective energy delivery to balance safety and efficacy in different anatomical zones.
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.